Page 405 - The Vasculitides, Volume 1: General Considerations and Systemic Vasculitis
P. 405
Dermatologic Aspects of Systemic Vasculitis 379
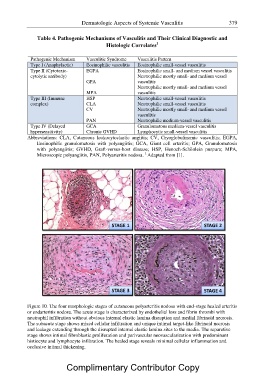
Table 4. Pathogenic Mechanisms of Vasculitis and Their Clinical Diagnostic and
Histologic Correlates1
Pathogenic Mechanism Vasculitic Syndrome Vasculitis Pattern
Type I (Anaphylactic) Eosinophilic vasculitis Eosinophilic small-vessel vasculitis
Type II (Cytotoxic- EGPA Eosinophilic small- and medium vessel vasculitis
cytolytic antibody) Neutrophilic mostly small- and medium vessel
GPA vasculitis
Neutrophilic mostly small- and medium vessel
MPA vasculitis
Type III (Immune HSP Neutrophilic small-vessel vasculitis
complex) CLA Neutrophilic small-vessel vasculitis
CV Neutrophilic mostly small- and medium vessel
vasculitis
PAN Neutrophilic medium-vessel vasculitis
Type IV (Delayed GCA Granulomatous medium-vessel vasculitis
hypersensitivity) Chronic GVHD Lymphocytic small-vessel vasculitis
Abbreviations: CLA, Cutaneous leukocytoclastic angiitis; CV, Cryoglobulinemic vasculitis; EGPA,
Eosinophilic granulomatosis with polyangiitis; GCA, Giant cell arteritis; GPA, Granulomatosis
with polyangiitis; GVHD, Graft-versus-host disease; HSP, Henoch-Sch?nlein purpura; MPA,
Microscopic polyangiitis, PAN, Polyarteritis nodosa. 1 Adapted from [1].
STAGE 1 STAGE 2
STAGE 3 STAGE 4
Figure 10. The four morphologic stages of cutaneoFuigsupreol1y0arteritis nodosa with end-stage healed arteritis
or endarteritis nodosa. The acute stage is characterized by endothelial loss and fibrin thrombi with
neutrophil infiltration without obvious internal elastic lamina disruption and medial fibrinoid necrosis.
The subacute stage shows mixed cellular infiltration and unique intimal target-like fibrinoid necrosis
and leakage extending through the disrupted internal elastic lamina sites to the media. The reparative
stage shows intimal fibroblastic proliferation and perivascular neovascularization with predominant
histiocyte and lymphocyte infiltration. The healed stage reveals minimal cellular inflammation and
occlusive intimal thickening.
Complimentary Contributor Copy