Page 272 - The Vasculitides, Volume 1: General Considerations and Systemic Vasculitis
P. 272
246 Christian Pagnoux and Gerard P. Cox
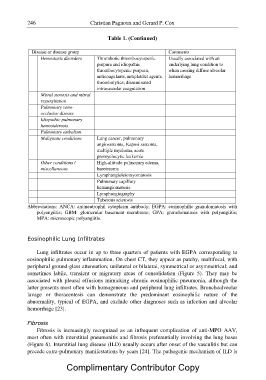
Table 1. (Continued)
Disease or disease group Comments
Hemostasis disorders Thrombotic thrombocytopenic Usually associated with an
purpura and idiopathic underlying lung condition to
thrombocytopenic purpura, when causing diffuse alveolar
anticoagulants, antiplatelet agents, hemorrhage
thrombolytics; disseminated
intravascular coagulation
Mitral stenosis and mitral
regurgitation
Pulmonary veno-
occlusive disease
Idiopathic pulmonary
hemosiderosis
Pulmonary embolism
Malignant conditions Lung cancer, pulmonary
angiosarcoma, Kaposi sarcoma,
multiple myeloma, acute
promyelocytic leukemia
Other conditions / High-altitude pulmonary edema,
miscellaneous barotrauma
Lymphangioleiomyomatosis
Pulmonary capillary
hemangiomatosis
Lymphangiography
Tuberous sclerosis
Abbreviations: ANCA: antineutrophil cytoplasm antibody; EGPA: eosinophilic granulomatosis with
polyangiitis; GBM: glomerular basement membrane; GPA: granulomatosis with polyangiitis;
MPA: microscopic polyangiitis.
Eosinophilic Lung Infiltrates
Lung infiltrates occur in up to three quarters of patients with EGPA corresponding to
eosinophilic pulmonary inflammation. On chest CT, they appear as patchy, multifocal, with
peripheral ground-glass attenuation; unilateral or bilateral, symmetrical or asymmetrical; and
sometimes labile, transient or migratory areas of consolidation (Figure 5). They may be
associated with pleural effusions mimicking chronic eosinophilic pneumonia, although the
latter presents most often with homogeneous and peripheral lung infiltrates. Bronchoalveolar
lavage or thoracentesis can demonstrate the predominant eosinophilic nature of the
abnormality, typical of EGPA, and exclude other diagnoses such as infection and alveolar
hemorrhage [23].
Fibrosis
Fibrosis is increasingly recognized as an infrequent complication of anti-MPO AAV,
most often with interstitial pneumonitis and fibrosis preferentially involving the lung bases
(Figure 6). Interstitial lung disease (ILD) usually occurs after onset of the vasculitis but can
precede extra-pulmonary manifestations by years [24]. The pathogenic mechanism of ILD is
Complimentary Contributor Copy