Page 154 - The Vasculitides, Volume 1: General Considerations and Systemic Vasculitis
P. 154
130 J. Charles Jennette, Ronald J. Falk and Adil. H. M. Gasim
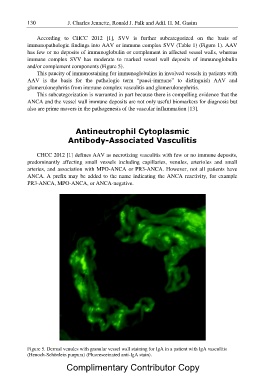
According to CHCC 2012 [1], SVV is further subcategorized on the basis of
immunopathologic findings into AAV or immune complex SVV (Table 1) (Figure 1). AAV
has few or no deposits of immunoglobulin or complement in affected vessel walls, whereas
immune complex SVV has moderate to marked vessel wall deposits of immunoglobulin
and/or complement components (Figure 5).
This paucity of immunostaining for immunoglobulins in involved vessels in patients with
AAV is the basis for the pathologic term “pauci-immune” to distinguish AAV and
glomerulonephritis from immune complex vasculitis and glomerulonephritis.
This subcategorization is warranted in part because there is compelling evidence that the
ANCA and the vessel wall immune deposits are not only useful biomarkers for diagnosis but
also are prime movers in the pathogenesis of the vascular inflammation [13].
Antineutrophil Cytoplasmic
Antibody-Associated Vasculitis
CHCC 2012 [1] defines AAV as necrotizing vasculitis with few or no immune deposits,
predominantly affecting small vessels including capillaries, venules, arterioles and small
arteries, and association with MPO-ANCA or PR3-ANCA. However, not all patients have
ANCA. A prefix may be added to the name indicating the ANCA reactivity, for example
PR3-ANCA, MPO-ANCA, or ANCA-negative.
Figure 5. Dermal venules with granular vessel wall staining for IgA in a patient with IgA vasculitis
(Henoch-Schönlein purpura) (Fluoresceinated anti-IgA stain).
Complimentary Contributor Copy