Page 203 - The Vasculitides, Volume 1: General Considerations and Systemic Vasculitis
P. 203
Classification and Pathogenicity of ANCA-Associated Vasculitis 179
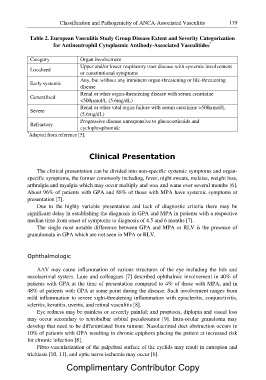
Table 2. European Vasculitis Study Group Disease Extent and Severity Categorization
for Antineutrophil Cytoplasmic Antibody-Associated Vasculitides*
Category Organ involvement
Localised Upper and/or lower respiratory tract disease with systemic involvement
or constitutional symptoms
Early systemic Any, but without any imminent organ-threatening or life-threatening
disease
Generalised Renal or other organ-threatening disease with serum creatinine
<500µmol/L (5.6mg/dL)
Severe Renal or other vital organ failure with serum creatinine >500µmol/L
(5.6mg/dL)
Refractory Progressive disease unresponsive to glucocorticoids and
cyclophosphamide
*Adapted from reference [5].
Clinical Presentation
The clinical presentation can be divided into non-specific systemic symptoms and organ-
specific symptoms, the former commonly including, fever, night sweats, malaise, weight loss,
arthralgia and myalgia which may occur multiply and wax and wane over several months [6].
About 96% of patients with GPA and 88% of those with MPA have systemic symptoms at
presentation [7].
Due to the highly variable presentation and lack of diagnostic criteria there may be
significant delay in establishing the diagnosis in GPA and MPA in patients with a respective
median time from onset of symptoms to diagnosis of 4.5 and 6 months [7].
The single most notable difference between GPA and MPA or RLV is the presence of
granulomata in GPA which are not seen in MPA or RLV.
Ophthalmologic
AAV may cause inflammation of various structures of the eye including the lids and
nasolacrimal system. Lane and colleagues [7] described ophthalmic involvement in 40% of
patients with GPA at the time of presentation compared to 4% of those with MPA; and in
48% of patients with GPA at some point during the disease. Such involvement ranges from
mild inflammation to severe sight-threatening inflammation with episcleritis, conjunctivitis,
scleritis, keratitis, uveitis, and retinal vasculitis [8].
Eye redness may be painless or severely painful; and proptosis, diplopia and visual loss
may occur secondary to retrobulbar orbital pseudotumor [9]. Intra-ocular granuloma may
develop that need to be differentiated from tumour. Nasolacrimal duct obstruction occurs in
10% of patients with GPA resulting in chronic epiphora placing the patient at increased risk
for chronic infection [8].
Fibro-vascularization of the palpebral surface of the eyelids may result in entropion and
trichiasis [10, 11], and optic nerve ischemia may occur [6].
Complimentary Contributor Copy